Abstract
Background
Monoclonal serum free light chains (sFLC) are detected in patients with B-cell proliferative disorders including multiple myeloma (MM) at diagnosis and disease relapse. Several previous studies demonstrated prognostic impact of the involved and uninvolved sFLC ratio (rFLC) in patients with newly diagnosed MM, patients with monoclonal gammopathy with undetermined significance, and smoldering MM. However, the prognostic impact of rFLC and differences between involved and uninvolved FLCs (dFLC) at the time of disease relapse have not been fully elucidated.
Patients and methods
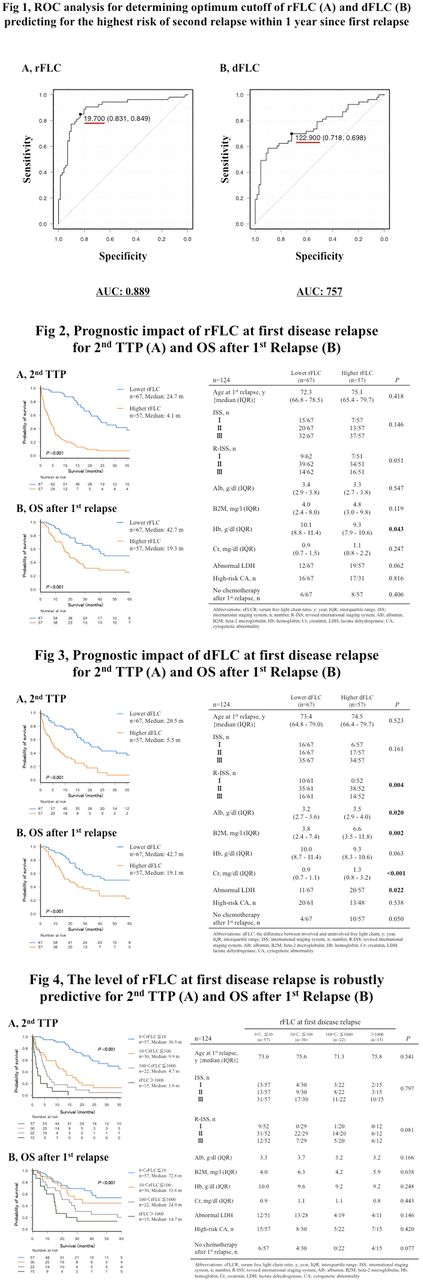
We identified consecutive patients with symptomatic MM, diagnosed and treated at Kameda Medical Center from January 2006 to April 2017. Patients who experienced initial relapse during June 2007 (the time where we began to routinely measure sFLC in MM patients) to April 2017 were identified. We reviewed background and outcome data from the electronic record. IMWG response criteria were used for assessing response and disease progression. rFLC was defined as involved FLC (iFLC) level divided by uninvolved FLC (uFLC) level. dFLC was calculated by subtracting uFLC from iFLC. Time to second progression (2nd TTP) and overall survival after first relapse (OS after 1st relapse) were defined as the time from the date of first progression to the date of second progression and death from any cause, respectively. Receiver operating characteristic (ROC) analysis determined optimal cutoff levels of rFLC and dFLC. We divided patients into high or low rFLC or dFLC, according to these cutoff levels. To clarify the relationship between rFLC increase at relapse and subsequent prognosis, patients were divided into 4 groups according to the rFLC levels: patients with rFLC >0 and ≤10, >10 and ≤100, >100 and ≤1000, and >1000.
Results
There were 240 patients diagnosed with symptomatic MM. Among them, 124 patients experienced disease relapse at least once during the observation period. Of the 124 patients, 97 were classified as having intact immunoglobulin MM and 27 had light chain MM. Median observation period from first relapse and age at first relapse of the 124 patients was 19.8 (range: 0.7 - 111.4) months (m) and 73.7 (range: 46.7 - 90.1) years, respectively. All patients received novel induction therapy agents. Using ROC analysis, we determined the optimal cutoff of rFLC and dFLC for predicting highest risk of second relapse within 1 year of first relapse as 19.7 and 122.9 mg/L, respectively. Patients with higher rFLC (n=57) had significantly shorter 2nd TTP and OS after 1st relapse than those with lower rFLC (n=67) (median 2nd TTP, 4.1 vs 24.7 m; P<0.001, and median OS after 1st relapse, 19.3 vs 42.7 m; P<0.001, respectively). Patients with higher dFLC (n=57) had significantly shorter 2nd TTP and OS after 1st relapse than those with lower rFLC (n=67) (median 2nd TTP, 5.5 vs 20.5 m; P<0.001, median OS after 1st relapse, 19.1 vs 42.7 m; P<0.001, respectively). Both 2nd TTP and OS after 1st relapse were significantly shorter when associated with increased rFLC levels. The median survival of patients with rFLC >0 and ≤10 (n=57), >10 and ≤100 (n=30), >100 and ≤1000 (n=22), and >1000 (n=15) were 30.5, 9.9, 4.7 and 1.6 m, respectively for 2nd TTP and 72.6, 33.6, 24.9 and 14.7 m respectively for OS after 1st relapse (both, P<0.001), whereas no significant difference was detected among the four risk groups of patients for age at first relapse, international staging system (ISS), revised ISS, the level of albumin, beta-2 microglobulin, creatinin, hemoglobin, lactate dehydrogenase abnormality, high-risk cytogenetic abnormality, or chemotherapy after first relapse.
Conclusion
At disease relapse, both rFLC and dFLC clearly identified different patient risk groups for subsequent prognosis. High rFLC and dFLC at relapse related to shorter 2nd TTP and OS after 1st relapse. Our data indicate that serial measurement of serum FLC assays may predict prognosis after relapse in patients with MM who receive novel agents and experience disease progression.
Kitadate: Kyowa Kirin: Research Funding; Eisai: Research Funding; Asahi Kasei: Research Funding; Pfizer: Research Funding; Otsuka: Research Funding; Chugai: Research Funding; Novartis: Research Funding; Fujimoto: Research Funding; Toyama kagaku: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.